Slide Show - What is Ulcerative Colitis?
Click here to take our SURVEY
Your feedback is important to us! We will use your feedback to develop future areas of content about IBD which will help other patients, caregivers and families.



*Please note: This slide show represents a visual interpretation and is not intended to provide, nor substitute as, medical and/or clinical advice.
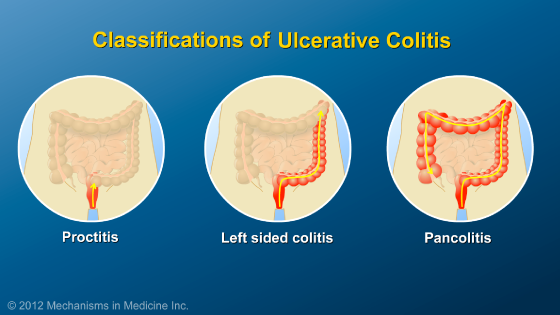
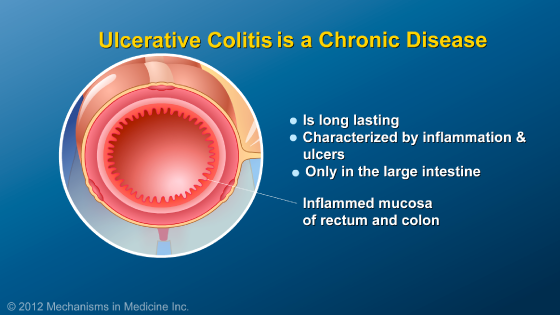
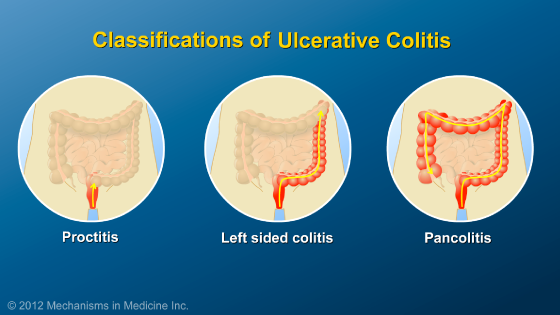
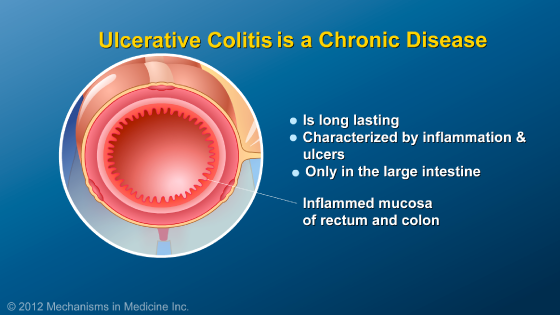
Ulcerative colitis is a chronic condition, characterized by inflammation and sores (ulcers) in the rectum and colon (large intestine). Ulcerative colitis can be distinguished based on how much of the large intestine is involved.
When ulcerative colitis involves only the rectum, it is referred to as “proctitis”. If the left side of the colon is involved, it is known as “left sided colitis”. When the entire colon is involved, it is known as “pancolitis”.
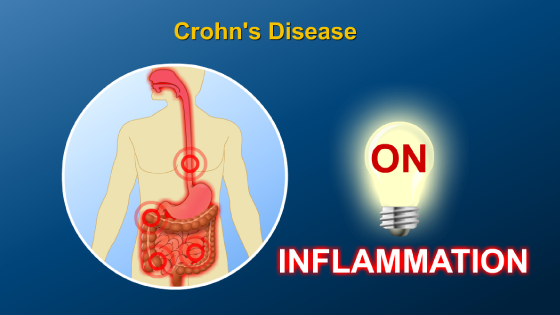
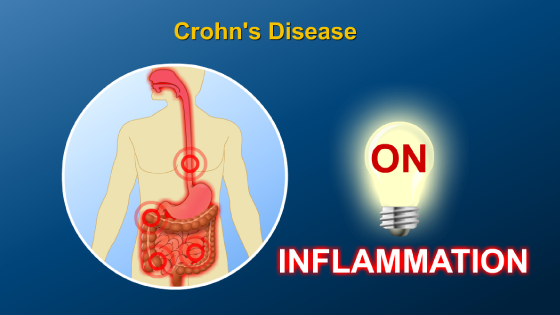
Ulcerative colitis is characterized by periods of time with active inflammation when the patient is experiencing symptoms, and periods of time when the inflammation is turned “off” and the patient feels well. We call these periods of wellness “remission”.
Ulcerative colitis is characterized by periods of time with active inflammation when the patient is experiencing symptoms, and periods of time when the inflammation is turned “off” and the patient feels well. We call these periods of wellness “remission”.
Many patients with ulcerative colitis have long periods of remission alternating with periods of active inflammation which are called “flares”. Some patients with ulcerative colitis have more severe flares than others.
Current thinking is that UC is caused by abnormal regulation of the immune system. The gastrointestinal tract (or GI tract) is frequently confronted with bacteria from our diet and environment
Although the cause of ulcerative colitis is not known, many factors can contribute to a person’s risk of having ulcerative colitis, but most can be thought of in three categories: genetic predisposition, environmental factors, and a dysregulated immune response in the GI tract, which causes the inflammation.
Environmental factors may include infections, smoking, and taking antibiotics or nonsteroidal anti-inflammatory drugs (NSAIDs).
In ulcerative colitis, inflammation appears within the colon, and the immune system works to combat the bacteria and viruses as it does with a cut on the surface of the skin.
However, the difference is that the immune system is not able to turn itself off after it rids the body of the bacteria or viruses, so the ulcers remain until they are treated with medicine or surgery.
This chronic inflammation is what causes the symptoms of ulcerative colitis.
In ulcerative colitis, the rectum (the last 6 inches of large intestine) is always involved. The inflammation may involve additional areas of the large intestine above this area. In some patients the inflammation may extend further up into the colon, and it is thought that in some patients the inflammation “extends” higher up over time.
Approximately half of patients who do not have the whole colon involved at the time of diagnosis eventually progress to more extensive disease, which may result in new symptoms or loss of response to an existing therapy.
Most of the symptoms of ulcerative colitis are related to inflammation of the rectum. When the rectum is inflamed, it is not able to store contents or distinguish gas from liquid.
Because of this, patients frequently feel the urge to run to the bathroom or fear that they will leak or have an accident.
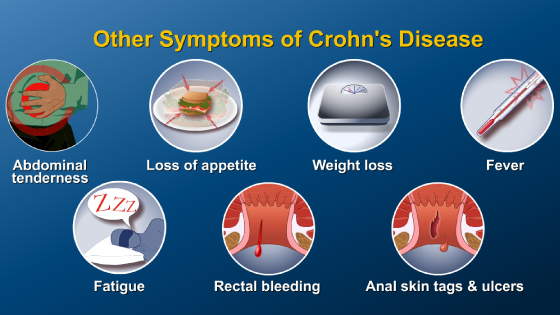
While bloody diarrhea tends to be the most frequently encountered problem, abdominal cramping is also common at the time of a bowel movement.
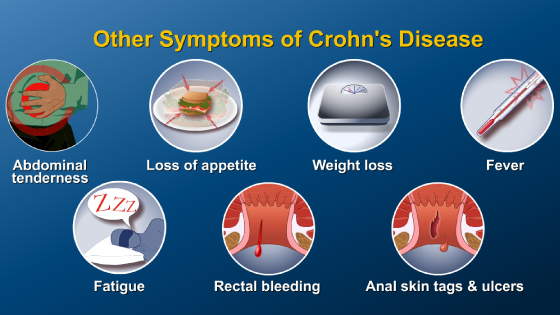
Other symptoms of ulcerative colitis can include frequent small stools, fatigue, low energy, and rarely, fever. Because the rectum is always involved in ulcerative colitis, patients usually experience similar symptoms regardless of how much of the colon is involved.
However, some patients may have more of the colon involved and tend to feel worse, bleed more, and be sicker.
In addition to symptoms involving the colon, ulcerative colitis can affect other parts of the body. Symptoms outside of the GI tract can include joint pain, liver inflammation, osteoporosis, skin problems, eye problems, mouth ulcers, and anemia.
Patients with ulcerative colitis should expect to lead normal lives. An important goal of the healthcare provider is to help people manage the disease, rather than having the disease manage them.
Click here to take our SURVEY
Your feedback is important to us! We will use your feedback to develop future areas of content about IBD which will help other patients, caregivers and families.



This educational activity has been developed by Imedex, LLC and Mechanisms in Medicine Inc.
Winner of the 7th Annual NAMEC Award
Best Practice in Collaboration Among CME Stakeholders
An Educational Collaborative with the
American College of Gastroenterology
This educational activity has been developed by
Imedex, LLC and Mechanisms in Medicine Inc.

This educational activity is supported by:






This website is part of the Animated Patient™ series developed by Mechanisms in Medicine Inc., to provide highly visual formats of learning for patients to improve their understanding, make informed decisions, and partner with their healthcare professionals for optimal outcomes.