*Please note: This slide show represents a visual interpretation and is not intended to provide, nor substitute as, medical and/or clinical advice.
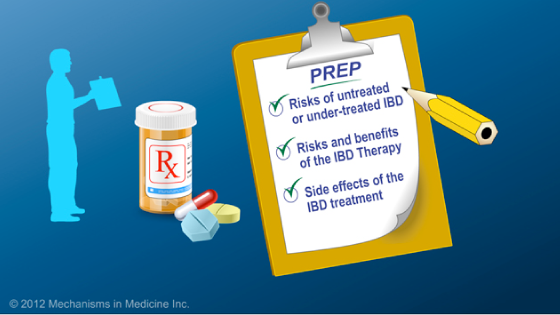
When discussing therapies to manage inflammatory bowel disease (IBD), patients and their doctors should consider both the risks of the disease (and likelihood medications can prevent those risks) and the risks of therapy.
Without medications, the chance that a patient would need surgery for Crohn’s disease within one year of diagnosis is 40%. That risk increases to 60% within 5 years, and to 70% after 10 years.
Therapy can help to establish and maintain disease control, reduce the frequency of relapse, reduce the chance of needing surgery or recurrence after surgery, and facilitate normal growth and development in children.
In order to improve quality of life, several therapies are available to treat IBD. The patient and their doctor should consider the potential benefits and risks of these treatments.
Medications that are typically used to treat Crohn’s disease include aminosalicylates, (which include mesalamine), antibiotics, corticosteroids, immunomodulators, and biologics. Patients should discuss which medication is right for them based on their individual disease location, severity and overall prognosis.
Mesalamine, or 5-ASAs, can be useful to treat mild to moderate cases of IBD involving the colon.
Mesalamines are among the safest agents used to treat IBD; however, some side effects are unpredictable and very uncommon. To monitor for rare side effects, patients should have a blood and urine test to check their kidney function every year.
Antibiotics, such as ciprofloxacin and metronidazole, are most commonly used to manage Crohn’s disease involving the perianal region and sometimes when the colon is inflamed. Antibiotics don’t work well for ulcerative colitis flares.
Corticosteroids can reduce inflammation quickly and inexpensively, but are not considered long-term solutions.
The reason why steroids are for short term use only is because of the side effects that are commonly seen. Examples of some common side effects include weight gain, moon facies and acne. Insomnia, high blood pressure, diabetes, osteoporosis, cataracts, irritability, depression, and growth delay in children with IBD is also possible.
Other medications used to treat IBD are the immunomodulators: 6-mercaptopurine (6-MP), azathioprine, and methotrexate. These are typically reserved for patients who are unable to discontinue steroids and need a therapy to maintain their disease under control for long term. These therapies are relatively inexpensive although they can take a considerable period of time – between 2 and 4 months – before a clear effect can be seen.
Some of the most common side effects with these drugs are allergic reactions (which occur in about 2 out of every 100 patients, or 2%), nausea in 2% of patients, abnormal liver tests in 2% of patients, pancreatitis in 3% of patients, and serious infections in 3% of patients. An extremely rare side effect of these therapies is non-Hodgkin’s lymphoma (which is cancer of the lymph nodes): 0.04% of patients, or 4 out of 10,000.
While these side effects can seem overwhelming, it is important to realize that 89% of patients can take these medications without having to stop them due to some side effect of the medication.
Other types of medications used to treat IBD are called anti-tumor necrosis agents or anti-TNF agents. The side effects of these medications can include infusion or injection site reactions, symptoms similar to lupus, and infections.
Overall, 90% of patients can take anti-TNF agents without having to stop them due to a side effect of the medication.
Understandably, looking at the side effects of these medications can be quite scary. However, it is important to understand what the risks are relative to other risks we face in our day to day lives.
To better understand how we can compare risks of side effects, the example of non-Hodgkin’s lymphoma is helpful. Non-Hodgkin’s lymphoma is a type of cancer. The risk of a patient with Crohn’s disease developing non-Hodgkin’s lymphoma is 2 out of 10,000 patients.
We can put this risk into perspective by looking at the chance of a Crohn’s patient developing non-Hodgkin’s lymphoma is 2 in 10,000 people – the same as the risk of dying due to a bicycle accident.
Looking at another risk of side effects, in patients with Crohn’s disease who receive a combination of anti-TNF agents and 6-mercaptopurine or azathioprine, the risk of developing non-Hodgkin’s lymphoma is 6 patients out of 10,000. Let’s also put this into perspective: It is more likely for a person to die from drowning than for this to occur.
Hopefully, the information presented here will help patients to more confidently analyze the risks and benefits associated with their IBD treatment options. As always, it is important for patients to discuss the potential benefits and risks of any drug they are taking with their doctors.
This slide show describes risks of inflammatory bowel disease (IBD) and risks/benefits of medication (5-ASAs, steroids, immunomodulators, & biologics).
-
Share with family and friends:
Click here to take our SURVEY
Your feedback is important to us! We will use your feedback to develop future areas of content about IBD which will help other patients, caregivers and families.